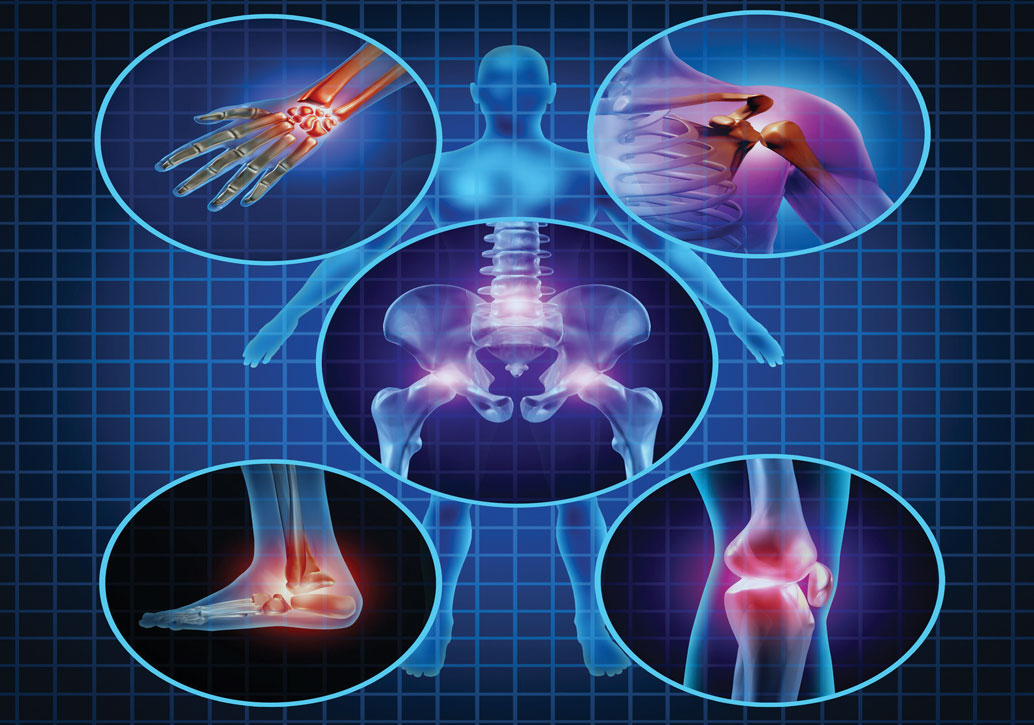
Arthritis is a form of joint disorder that literally means inflammation of a joint (from the Greek arthro, meaning joint, plus itis meaning inflammation). Scores of causes of arthritis primarily affect older people, but the most common is osteoarthritis. This condition is recognizable by pain, swelling and limited movement in one or more joints. It is especially disabling when it occurs in the large joints of the body, such as the knees and hips.
Arthritis is a form of joint disorder that literally means inflammation of a joint (from the Greek arthro, meaning joint, plus itis meaning inflammation). Scores of causes of arthritis primarily affect older people, but the most common is osteoarthritis. This condition is recognizable by pain, swelling and limited movement in one or more joints. It is especially disabling when it occurs in the large joints of the body, such as the knees and hips.
By Dr. Michael Gordon
The difficulty with labelling all causes of pain in older people as “arthritis” is that there is a tendency to ignore its seriousness. But for many, even relatively mild osteoarthritis cannot be ignored. According to The Arthritis Society, 4.5 million, or one in six, Canadians aged 15 years and older report having arthritis. By 2031, approximately seven million Canadians (one in five) are expected to have arthritis. When the condition affects more than one joint, such as both knees and a hip, it often severely impacts a person’s comfort, not to mention their independence and ability to carry out normal activities such as dressing, shopping, bathing and walking. Such discomfort has severe implications for a person’s quality of life.
For those with “arthritis” affecting one or more joints and who are suffering pain and disability, treatment should include analgesic medications, even if other interventions are proposed. The medication prescribed should preferably be one that is tolerated,
has few deleterious effects and can be taken over a long period of time.
Lifestyle modification may also be useful. An exercise program can increase the movements of affected joints without causing further damage and pain. Any new program may require professional supervision from a qualified person who understands the needs, demands and risks of exercise in older individuals. Dietary changes can be helpful in some people, particularly if the compromised joint is being asked to carry excess weight. In some individuals and situations, the only real long-term option is surgery on the affected joints. This can mean joint replacement surgery, which has advanced substantially over the past decade.
Whichever course a patient decides on, a multi-professional assessment is often worthwhile. This should encompass not only the specific joints involved, but all the other factors that may play a role in comfort and function. Experts in the fields of physiotherapy and occupational therapy can help ensure your safety when you are not able to carry out all your self-care tasks easily, as well as prescribing gait assessment and exercises to improve balance. Some programs include activities that are done alone, while others involve group settings or venues that can be soothing to the joint discomfort. An example is the use of so-called “therapeutic pools,” where the water is of the right warm temperature and exercises are supervised to maximize benefit and decrease the risk of excessive demands on the affected joints.
Above all, patients should not give up hope. Getting good advice and finding a program and treatments that meet physical needs, and personality preferences and choices, is possible.
Dr. Michael Gordon is Medical Program Director of Palliative Care at Baycrest Geriatric Health Care System.